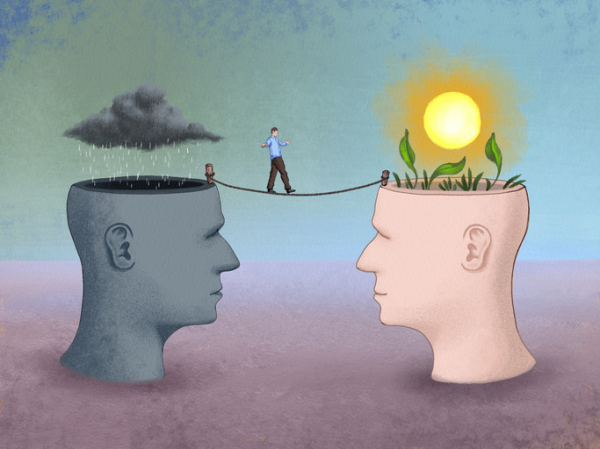
Nantucket, a beautiful, 14-mile-long island off the coast of Massachusetts, has a 40-point resiliency plan to help withstand the buffeting seas surrounding it as climate change takes a toll. Perhaps we can all benefit from creating individual resilience plans to help handle the big and small issues that erode our sense of well-being. But what is resilience and how do you cultivate it?
What is resilience?
Resilience is a psychological response that helps you adapt to life’s difficulties and seek a path forward through challenges.
“It’s a flexible mindset that helps you adapt, think critically, and stay focused on your values and what matters most,” says Luana Marques, an associate professor of psychiatry at Harvard Medical School.
While everyone has the ability to be resilient, your capacity for resilience can take a beating over time from chronic stress, perhaps from financial instability or staying in a job you dislike. The longer you’re in that situation, the harder it becomes to cope with it.
Fortunately, it’s possible to cultivate resilience. To do so, it helps to exercise resiliency skills as often as possible, even for minor stressors. Marques recommends the following strategies.
Shift your thoughts
In stressful situations, try to balance out your thoughts by adopting a broader perspective. “This will help you stop using the emotional part of your brain and start using the thinking part of your brain. For example, if you’re asking for a raise and your brain says you won’t get it, think about the things you’ve done in your job that are worthy of a raise. You’ll slow down the emotional response and shift your mindset from anxious to action,” Marques says.
Approach what you want
“When you’re anxious, stressed, or burned out, you tend to avoid things that make you uncomfortable. That can make you feel stuck,” Marques says. “What you need to do is get out of your comfort zone and take a step toward the thing you want, in spite of fear.”
For example: If you’re afraid of giving a presentation, create a PowerPoint and practice it with colleagues. If you’re having conflict at home, don’t walk away from your partner — schedule time to talk about what’s making you upset.
Align actions with your values
“Stress happens when your actions are not aligned with your values — the things that matter most to you or bring you joy. For example, you might feel stressed if you care most about your family but can’t be there for dinner, or care most about your health but drink a lot,” Marques says.
She suggests that you identify your top three values and make sure your daily actions align with them. If being with family is one of the three, make your time with them a priority — perhaps find a way to join them for a daily meal. If you get joy from a clean house, make daily tidying a priority.
Tips for success
Practice the shift, approach, and align strategies throughout the week. “One trick I use is looking at my calendar on Sunday and checking if my actions for the week are aligned with my values. If they aren’t, I try to change things around,” Marques says.
It’s also important to live as healthy a lifestyle as possible, which will help keep your brain functioning at its best.
Healthy lifestyle habits include:
- getting seven to nine hours of sleep per night
- following a healthy diet, such as a Mediterranean-style diet
- aiming for at least 150 minutes of moderate-intensity activities (such as brisk walking) each week — and adding on strength training at least twice a week
- if you drink alcohol, limiting yourself to no more than one drink per day for women and two drinks per day for men
- not smoking
- staying socially connected, whether in person, by phone or video calls, social media, or even text messages.
Need resilience training?
Even the best athletes have coaches, and you might benefit from resilience training.
Consider taking an online course, such as this one developed by Luana Marques. Or maybe turn to a therapist online or in person for help. Look for someone who specializes in cognitive behavioral therapy, which guides you to redirect negative thoughts to positive or productive ones.
Just don’t put off building resilience. Practicing as you face day-to-day stresses will help you learn skills to help navigate when dark clouds roll in and seas get rough.
About the Author

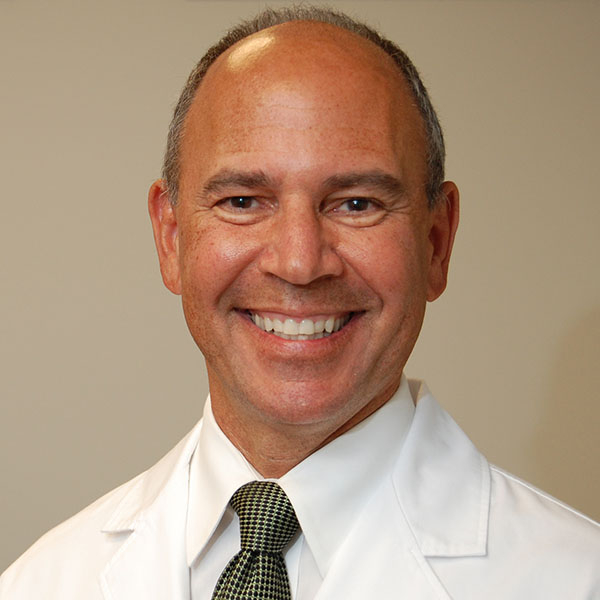
Heidi Godman, Executive Editor, Harvard Health Letter
Heidi Godman is the executive editor of the Harvard Health Letter. Before coming to the Health Letter, she was an award-winning television news anchor and medical reporter for 25 years. Heidi was named a journalism fellow … See Full Bio View all posts by Heidi Godman
About the Reviewer
Howard E. LeWine, MD, Chief Medical Editor, Harvard Health Publishing
Dr. Howard LeWine is a practicing internist at Brigham and Women’s Hospital in Boston, Chief Medical Editor at Harvard Health Publishing, and editor in chief of Harvard Men’s Health Watch. See Full Bio View all posts by Howard E. LeWine, MD